Chronic pain
Definition of pain
Pain is a complex sensation similar to a feeling. Pain is always subjective; it cannot be measured or proven and also not rebutted. Since the 1970s there has been an official definition by the International Association for the Study of Pain which applies for acute and also for chronic pain:
"Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage."
The definition follows the bio-psycho-social model of disease. This model describes that disease – and therefore also pain – is not exclusively caused by physical changes but also dysfunction, emotional, mental or social problems and disruptions can cause pain and disease. The above definition of pain therefore dismisses the causal link of damage and pain. This means that pain is not necessarily caused by an objective damage of tissue but that a subjective sensation of such damage is sufficient.
Acute pain
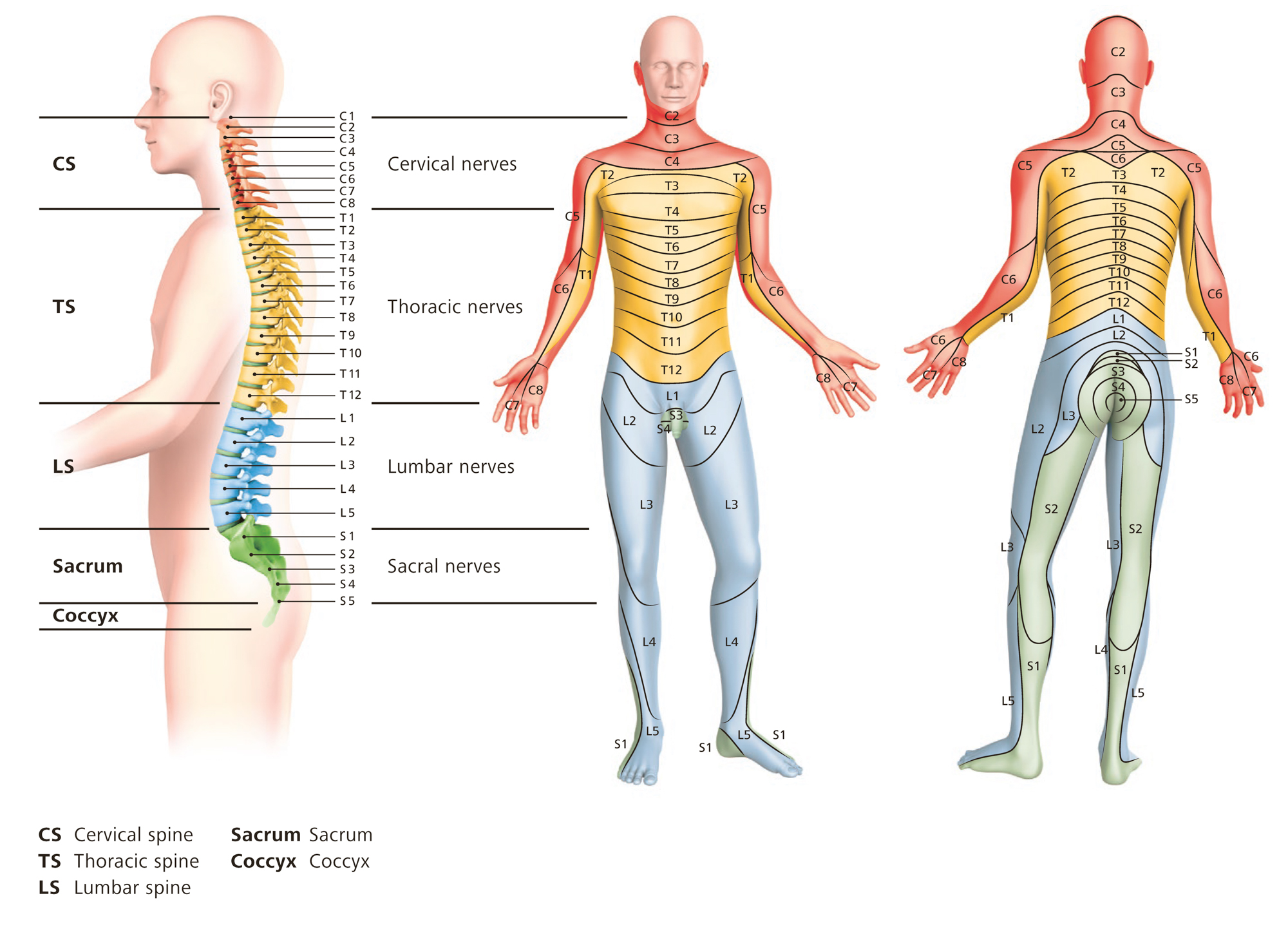
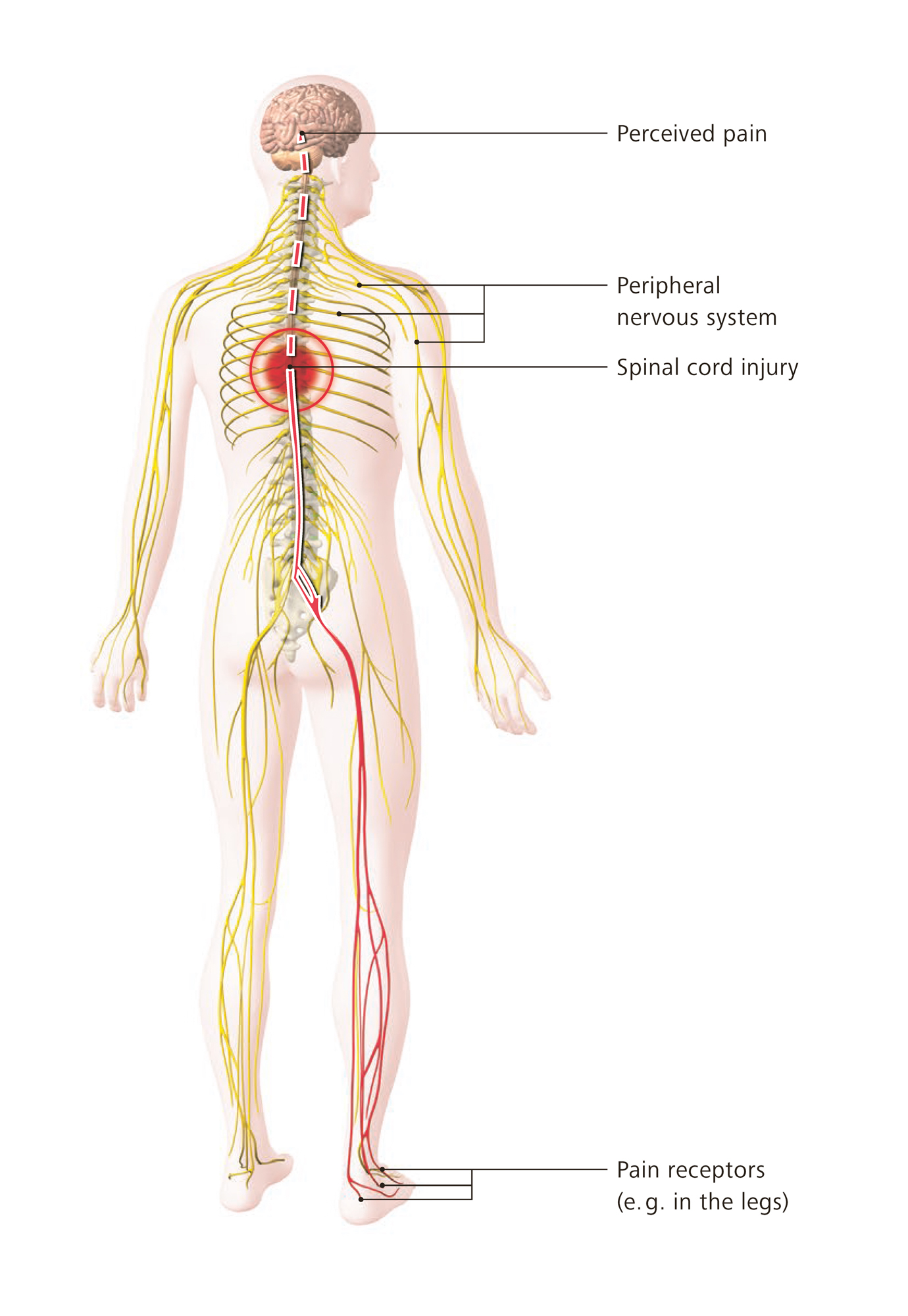
In case of acute pain receptors – or, simplified, microphones or call buttons – are activated inside the body which forward their information via the spinal cord and many interfaces to the central nervous system, our brain. Inside the brain this information is processed in a complex way. The result of these processes may be the sensation of pain combined with a certain characteristic (burning, stabbing, pulling, throbbing etc.) and a more or less exact location within the body. Pain can, however, also be suppressed by the brain, e.g. when we are distracted, tense or concentrating on an interesting work or more important tasks (such as fleeing a danger, shock after an accident).
Acute pain has a warning function. The removal of the cause, treatment of the injuries or the underlying disease eases the pain mostly fast and sustainably. Painkillers usually work well.
Chronic pain
Acute pain can turn into chronic pain. Chronic associated with pain does not only mean "long lasting" or "existing for a long time". Chronic pain also includes the interrelatedness of various factors. Signs for pain that is becoming chronic are that the symptoms are spreading on the physical level – the area affected by pain is extending, more areas of pain develop – but also on the mental-emotional level and in social life problems can occur.
Chronic pain can best be prevented if it is treated early and appropriately. If it targeted and usually well working treatments have hardly any influence on the pain, it should be checked whether it is still an acute, simple pain and also other influences should be taken into consideration.
Frequent chronic pain problems are:
- Headache
- Back pain
- Neck pain
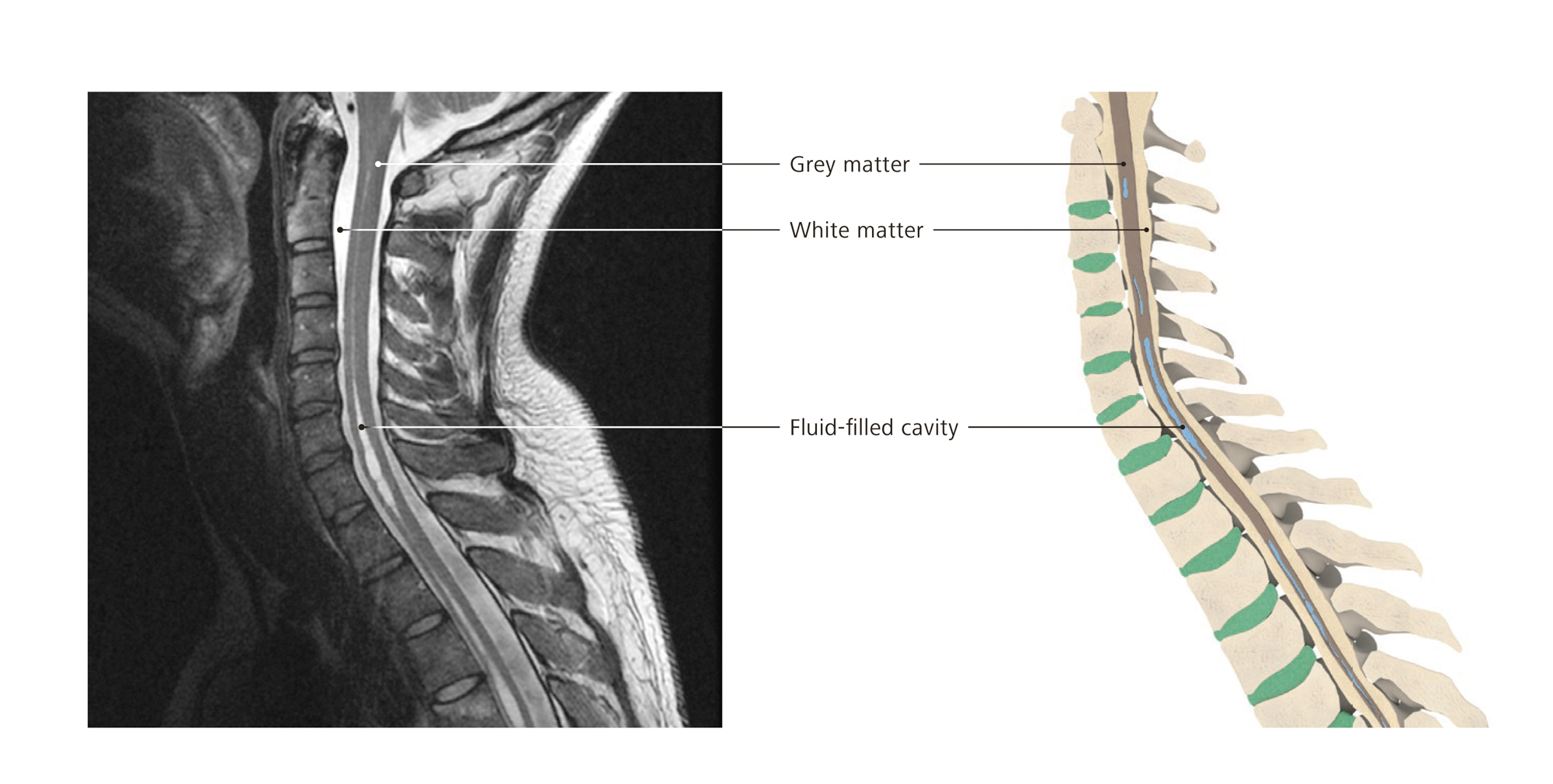
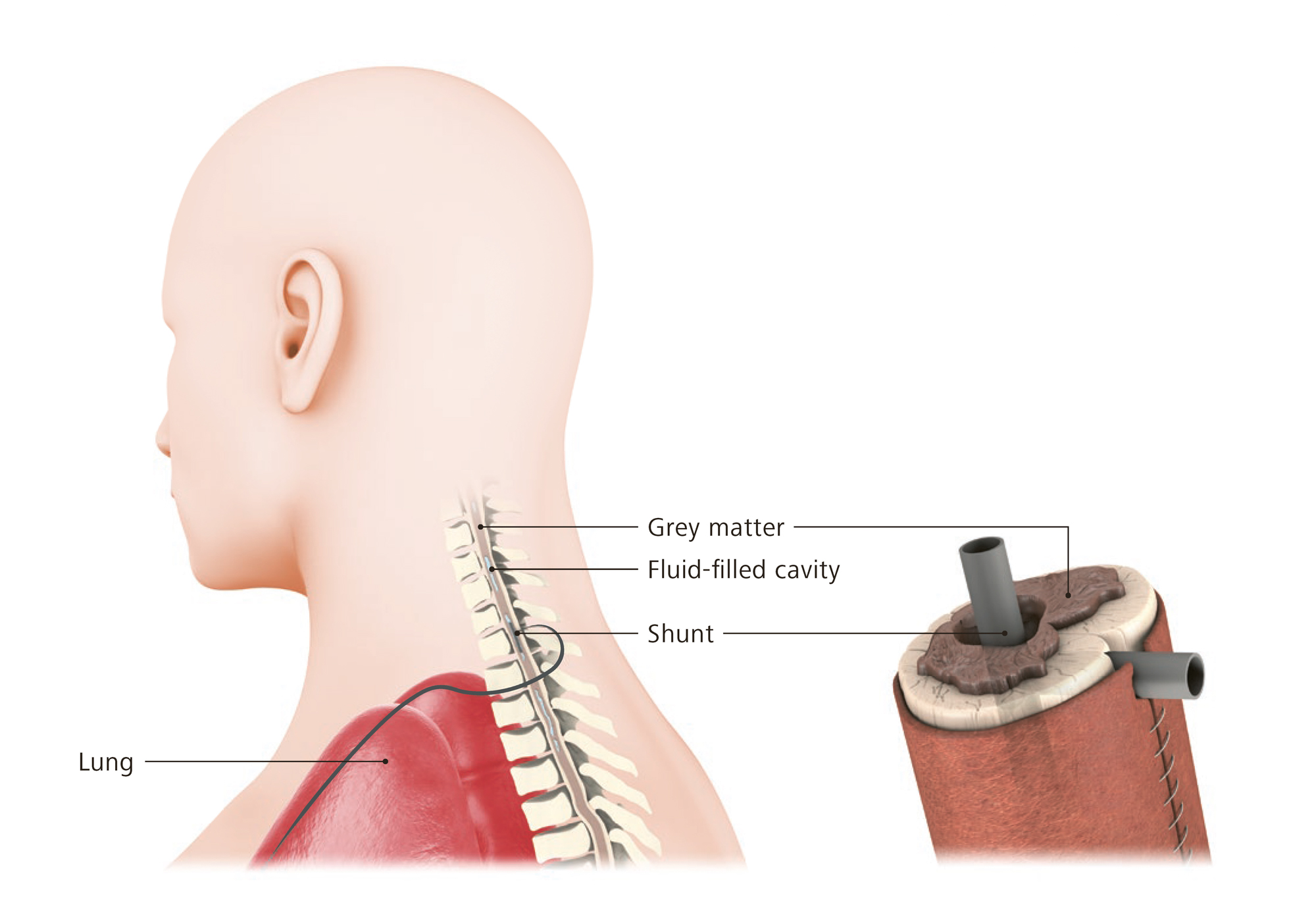
- Neuropathic pain (caused by damage of the nervous system such as spinal cord injury)
- Multilocular pain (i.e. at several locations) or extended (i.e. covering a larger body area) chronic pain (e.g. fibromyalgia)
In total about 16% of the persons residing in Switzerland are suffering from chronic pain, i.e. one in six. Persons with spinal cord injury suffer from chronic pain more frequently, often in combination with muscle spasticity. Most of them do not receive sufficient care and continue to suffer.

Causes and triggers
Pain can be versatile and each patient has a different perception of pain – as manifold can be the causes that trigger pain and they are often the beginning of several years of experiencing pain. Often the triggers occur at a time when the patient was in a difficult situation in life or has reached a turning point. Also previous injuries, experiences of violence or ongoing mental or social burdens may constitute weak points that may promote such a development.
Chronic pain, as generally recognized, can only be understood on the basis of a bio-psycho-social model of disease. The various parts may have a different significance from case to case. Chronic pain is often comes with a depressive mood, sometimes fear and often sleep disorders. In each case it needs to be examined whether sleep disorders has existed before (and may therefore have promoted the development of chronic pain) or whether they are co-existing without having an influence on the pain or whether they are the consequence of chronic pain. In each case they need to be treated in the context of a pain therapy.
Impact on the quality of life
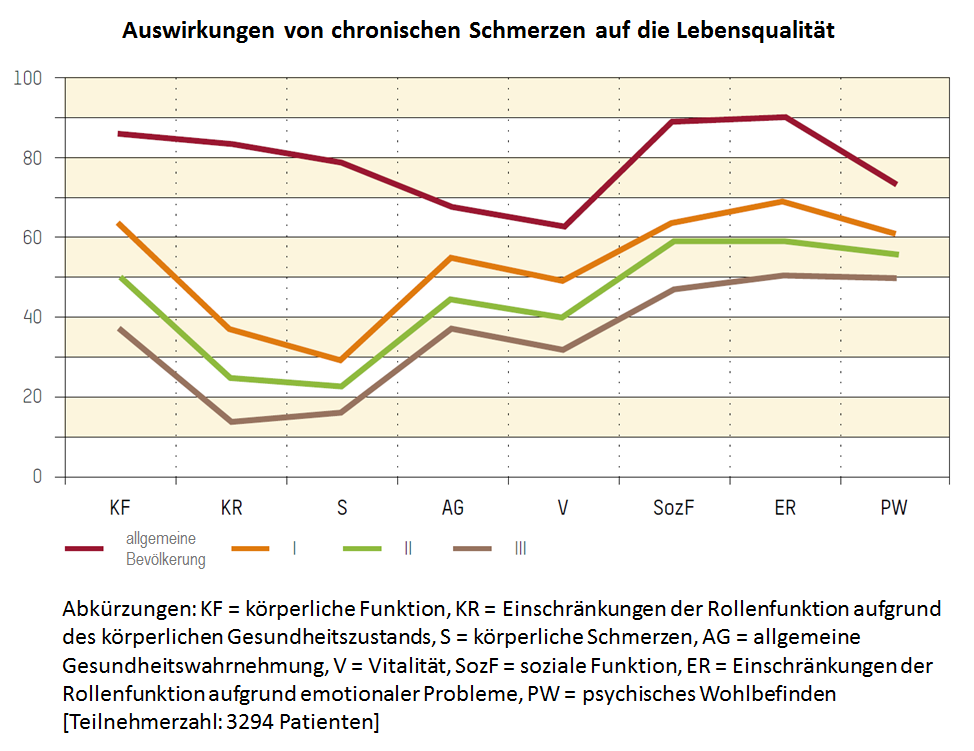
Research in the field quality of life was able to show that chronic pain affects a person in his/her entirety and all areas of life.
Self-assessment of health related quality of life with the SF-36 (short form 36), results in relation to pain chronification. The red curve shows the standard values of a representative sample of the general population. The orange curve "I" shows the results for patients with low chronified pain, the green curve "I" shows the values with a medium pain chronificiation and the brown curve "III" shows a high pain chronification (Mainz Pain Staging(MPSS) by Gerbershagen) [Resource: Gerbershagen HU, Lindena G, Korb J, Kramer S. Gesundheitsbezogene Lebensqualität bei Patienten mit chronischen Schmerzen. Der Schmerz. 2002;16(4),271-84.]
The diagram clearly shows that patients with an increasing pain chronification are limited in all enquired areas because of their chronic pain. Localization of the pain does not play a significant role in this context.
Diagnosis and treatment
In order to detect and diagnose chronic pain a team of specialists is necessary. An orthopedist, for example, is not able to competently assess the mood of a patient and make a psychiatric diagnosis; a social worker is not able to assess the performance of the patient, his/her limitations and resources; and a psychiatrist or psychologist cannot evaluate the degree of physical damage and the therapeutic possibilities (e.g. through physiotherapy). Therefore to assess the complexity of a patient and his/her situation, a team of pain specialists is necessary who exchange their assessments and findings and then coordinate further treatment measures. Gold standard for the treatment of chronic pain therefore is an interdisciplinary (i.e. across the disciplines) and multimodal (i.e. in different ways) pain therapy.
The success of the therapy strongly depends on the cooperation of the patient, from the anamnesis to the motivation and participation in the treatment. Generally the pain patient does not only get a diagnosis but a list of factors that causes and maintain pain. Pain is a combination of factors and gives expression to many things such as disease, suffering, limitations, suffered injustice and much more.
If possible the therapy takes place within a group since this allows the participants to support and learn from each other. In order for the group to be harmonious and for the group treatment to be successful a thorough selection of patients is necessary.
Swiss Paraplegic Centre in Nottwil, Switzerland, has the Centre for Pain Medicine, a specialist department for the treatment of acute and chronic pain. This is where outpatients and inpatients receive the best-possible examination of their pain problem and an accordingly designed treatment – see https://www.paraplegie.ch/spz/en/centre-pain-medicine-nottwil.
Useful links:
- An instructive video about how to deal with pain can be found here: www.youtube.com/watch?v=5KrUL8tOaQs.
- As a recently founded organization, "Schmerzliga Schweiz" offers information and capacity building (in German).
- A list of pain specialists with the certification "Pain specialist SASP" can be found on the website of the "Swiss Association for the Study of Pain" (SASP): www.pain.ch (in German and French).
About the author:
- Dr. med. André Ljutow, MSc, is leading the Centre for Pain Medicine, one of the biggest interdisciplinary specialist units for pain of the German-speaking countries. As "Pain specialist SASP" with numerous other international qualifications, Dr. med. Ljutow is currently also president of the Swiss Association for the Study of Pain. Furthermore, in his role on the scientific advisory board, he is working on the creation of a self-help organization for pain patients of "Schmerzliga Schweiz".
Skin and pressure sores
What causes pressure sores?
Long-lasting pressure or also brief, strong pressure on one part of the skin can cause a decrease in blood flow inside the tissue. The skin presents red spots that do not turn white when pressing. Skin hardens if it is repeatedly exposed to strain at the same point.
This reddening of the skin is caused by dead cells and requires decompression. The strain needs to be alleviated. This happens specifically to body parts that are paralysed and have no sensibility. Skin often reddens in combination with shear forces and rubbing.

What are shear forces?
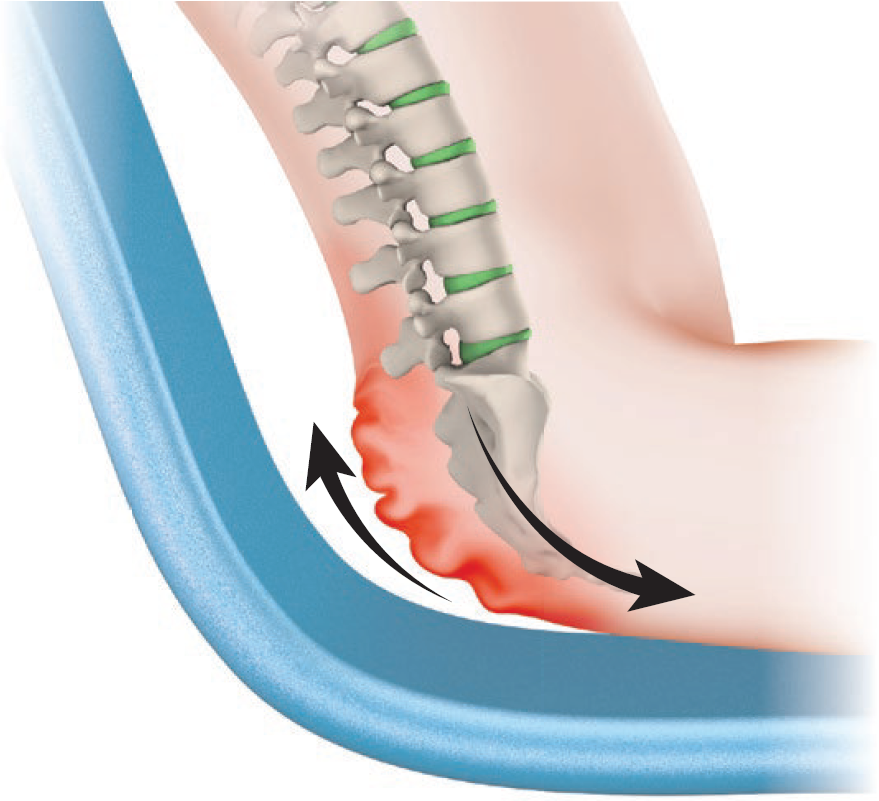
Shear forces occur when tissue is moved in opposite directions. Slow pushing or pulling of the various tissue layers causes micro injuries.
Shear forces occur when sitting in bed or when sliding over onto the wheelchair or shower wheelchair, etc.

When should the skin be checked?
The skin must be checked at least twice per day: in the morning during your personal hygiene, and at night when going to bed.
Additional skin checks are important …
… after sitting or lying on a new or unaccustomed surface
- New mattress or bedding material at home
- Unfamiliar mattress in a hotel, at friends’, in hospital, etc.
- New wheelchair or cushion
- New/unfamiliar shower seat or shower wheelchair
- Sports devices such as a monoski, handbike, speed wheelchair, etc.
- When travelling: seats on airplanes and buses, etc.
- Dentist’s chair, examination stretcher, x-ray stretcher, etc.
- Long car journeys
… after wearing new clothes and shoes
- Trousers with thick seams
… during a health condition or after an accident
- Fever, flu – attention: fever makes the skin much more sensitive!
- Diarrhoea
- Increased spasticity
- After falls
… when there are skin changes
- Swellings
- Dry skin – cracked skin, scaly skin
- Calluses
- Hard skin
… in a hot climate
- When perspiring profusely
The most important way to prevent pressure sores is to frequently check skin via visual examination and palpation:
Feeling and assessing
- Press the reddened part of the skin with your finger.
- If the spot disappears (whitish colour for 1–2 seconds), further damage can be avoided by relieving this part of the skin.
- If this part stays red, the skin is damaged and the condition is called decubitus. It is necessary to consistently relieve this part of the skin for a longer period.
- If hard skin, scabs or blisters have formed, the decubitus is deeply rooted and requires urgent treatment by a doctor.
What do I need to do in the case of pressure sores?
If reddening occurs, ease the pressure on the affected area of skin immediately until the skin has recovered. The further the pressure ulcer has progressed, the longer it will take to recover.
If an erythema can no longer be pressed away, more time is needed for the skin to recover. If the pressure ulcer occurs at a spot that is not affected when sitting in the wheelchair, it is possible to use the wheelchair during the day. However, more frequent periods of relief should be practised. If there is pressure on the affected part, it is necessary to lie in bed with frequent repositioning.
Attention: The coccyx area can also come under pressure when you are sitting in a wheelchair – shear forces.
The longer a pressure sore remains untreated, the deeper the decubitus will be and the longer the recovery period. It is not recommended to treat the wound by oneself over a longer period. Having it checked and treated by a GP or an outpatient care service helps to avoid complications.
How can I avoid pressure sores?
- Through regular relief of pressure or movement of the weight when sitting in a wheelchair – lifting, leaning to the side or ahead, tilting the wheelchair (roughly every 20 minutes)
- Pressure relief in bed by shifting into various positions – to the side, prone position
- Avoid sitting or lying by mistake on objects that can cause pressure ulcers – buttons, cell phones, etc.
- Crease-free bed sheets, suitable clothes without studs, buttons or thick seams on the buttocks or back
- By sitting on adapted cushions, if possible – on an airplane, bus, car, etc.
- Sit on a padded surface for personal hygiene: toilet seat, soft shower seat and shower wheelchair surface
If I notice a reddening at the buttocks using a mirror and cannot check myself if it can be pressed away, what can I do?
Family or a care service can hold the mirror for you or check your skin.
What do I do if I am unsure about my assessment of the reddened part?
Don’t hesitate to see your GP or ask an outpatient care service for help.
What can I do if I notice that my mattress is causing pressure sores repeatedly?
Check the age and condition of the mattress. You may have to get a softer mattress. There are various anti-decubitis mattresses available on the market. They can frequently be hired from companies on a trial basis. Ask your local SCI centre which mattresses are suitable.
Risks when living with limited sensitivity
How do we define sensitivity?
With sensitivity, we mean our fifth sense, namely feeling. Different from the other four senses, sensitivity is not perceived through a sensory organ such as vision is through the eyes. Our sensory system retrieves information from numerous nerve endings and receptors1 that are spread all over our body. This system gives us feedback from our body through pressure, stretching, vibration, temperature or pain. This feedback comes from different places: from the mucous membranes, the inner organs or the muscular / skeletal system (position of the joints, flexion of muscles).
This sensitivity is an important warning system of our body. If there is no or only partial sensitivity, we are not receiving information that would make us aware of hazards. Due to the limited sensitivity of people with spinal cord injury, this important warning mechanism is disabled, which can lead to various complications.
Risks due to limited or non-existent sensitivity
Pressure sores
As a result of limited or non-existent sensitivity, the risk of pressure sores is particularly great for people with spinal cord injuries.
Burns through heat therapy and the touching of hot objects or surfaces
Heat therapy is one of the oldest medical treatments and is used in conventional Western medicine as well as in natural medicine. Since it is used in the home environment, nearly everybody knows it: it includes a number of different applications such as hot-water bottles, cherry pit pads, heating pads and blankets, red light therapy, warm compresses and heat packs. Usually heat applications are perceived as comfortable, relaxing and revitalizing. However, using heat applications can be dangerous if the perception of heat is limited because this can cause burnings and scalding.
Furthermore, there are many everyday situations in which we come into contact with hot objects and surfaces. If the person’s ability to sense the heat is eliminated or limited, one has to be especially careful with:
- Taking a shower or a bath (watch out for changing water temperatures!
- Sink drainage
- Heating pads or hot-water bottles
- Carrying hot objects on the legs (you need protection between the object and the legs, e.g. use a tray with equalising padding.)
- Surfaces that retain heat (deck chair, sand, etc.)

Sun
The perception of heat and cold is impaired when sensitivity is limited. This may lead to hyperthermia or hypothermia of the body. People with a high spinal cord injury often feel cold and therefore dress overly warm and enjoy the warmth of the sun.
However, the sun also has its drawbacks. UV radiation can damage the skin (sunburn), and heat can lead to an overheating of the body (sunstroke). Excessive sunbathing speeds up the ageing process of our skin and promotes several other skin changes – it may even cause skin cancer.
Check your skin for alterations after spending time outside. Good sun protection (hat, sunglasses and sunscreen) is recommended.

Regulation of body temperature
Humans regulate their body temperature by sweating, among other things. People usually start to sweat at air temperatures just over 30°C. People with spinal cord injury are only able to sweat as a regulating measure in those areas of the body that are not paralysed. This means that especially tetraplegics have a considerably limited ability to regulate their body temperature, which is insufficient to keep it within a normal range when they expose themselves to high temperatures.
Due to the spinal cord injury, the autonomous nervous system can no longer control the mechanisms responsible for our temperature regulation (heat production and heat loss). These mechanisms include blood circulation in the skin, sweating, shivering and directing the blood from the abdominal organs towards the muscles. This may result in a decrease in body temperature (hypothermia) or an excessive elevation (hyperthermia). These issues may be caused by high room temperatures, intense sun radiation or wrong clothing. People with tetraplegia therefore have to pay special attention to ambient temperatures. They need to be especially careful when travelling to very hot countries but also during the summer time in Switzerland.
The following points are important for tetraplegics but also for people with paraplegia:
Fluid loss
Increased sweating requires increased fluid intake. As a general rule, the bladder should excrete at least 1.5 litres of urine per day. This helps to prevent thromboses and urinary tract infections.
Thromboses
The risk of thrombosis is increased during the hot season. Adequate fluid intake and compression stockings are the best possible prophylaxis. It is therefore important to check the legs for rashes, overheating, swelling and oedemas on a daily basis, because these are the first signs of thrombosis.
Pressure sores
Sweating causes damp skin and thus increases the risk of pressure sores. Pressure relief in the wheelchair is therefore important in order to prevent pressure sores. Damp clothes need to be changed and the skin check should never be forgotten.
Medications
People who are taking anticholinergics such as Ditropan® (for the treatment of an overactive bladder) or Buscopan® (against stomach cramps and spastic constipation) only perspire to a limited extent and therefore need to be particularly careful when being exposed to the sun. It is also important to check the package information leaflet to see if taking these drugs increases photosensitivity.
What to do on hot summer days:
- Take along a spray bottle filled with water to spray on your body in the case of hyperthermia – this makes up for the limited perspiration.
- Always wear a hat
- Drink plenty of water
- Avoid heat
- Wear light clothing
- Use a mobile fan

Also hypothermia may have severe physical consequences and can even lead to unconsciousness. It is therefore very important to be especially careful when staying outside for a longer period of time, also during the winter time, for instance when going for a stroll or skiing.
What can I do when I notice that I am overheating?
Spraying yourself with cold water (e.g. with a spray bottle) may be very efficient. Also make sure you drink enough. In general you should avoid strong and direct sunlight.
Are electric heating pads better than hot-water bottles?
Electric heating pads can also become very hot and therefore you need to be very careful about where you use them. Generally, you should use them only in those areas that show sensitivity.
Is it still possible for people with tetraplegia to travel to countries with a hot climate?
Yes, if you follow the above-mentioned recommendations, it should be possible. However, not everyone can withstand heat equally well. If the heat causes blood pressure problems, isotonic drinks might help.
1 specialised cell that transmits stimuli
ReadContractures
What are contractures and how do they develop?
Contractures are shortenings of muscles, tendons or ligaments that have a limiting effect on the movements of the joints. The normal ability to move a joint is lost. Contractures are frequently attributable to the patient’s positioning. They occur when muscles and joints are not stretched or moved often enough. If, for example, the knees are permanently bent, the muscles that are responsible for extending the knee joints will shorten. As a result, the legs can no longer be fully extended.
Contractures can also be caused by strong spasticity and spasms, as well as restricted movements in joints, e.g. arthritis.
Where can restrictions in movement caused by contractures be seen most frequently?
In principle, contractures in all joints can lead to restricted movement. However, they generally occur at the extremities. When it comes to feet, people talk in terms of equinus feet or claw toes. In claw toes, the toes bend down and cannot be straightened.
Like the legs, people’s arms are also affected by contractures, specifically their shoulders, elbows, wrists and finger joints. People with tetraplegia are at a particularly high risk. However, contractures may also lead to a restriction in head movement.
How can contractures be avoided?
Contractures can be avoided by moving arms and legs actively or passively and by changing the body position frequently. Changing position can prevent contractures.
Why is it important to avoid contractures?
Movement restrictions in arms and legs make everyday life more difficult. Transferring oneself and personal hygiene become more difficult, and a lack of ability to move the arms can decrease independence. If contractures make it difficult to change the patient’s position, this may lead to pressure sores as the pressure cannot be alternated around various areas of the body.

If positioning measures are not performed consistently and correctly, contractures may develop quickly and treating them might take a long time.
After being released from hospital, do I need to go on with equinus foot prophylaxis?
Normally not. If the feet are in the right position (min. 90° angle = 0° position in the ankle) during mobilization (more than 6 hours) and upright training is done, no equinus foot prophylaxis is necessary in bed. However, should the situation change, e.g. through increased spasticity, it needs to be reassessed whether equinus foot prophylaxis becomes necessary.
What happens if I rarely wear shoes in the wheelchair or not at all?
The footrests on the wheelchair are normally too narrow for the toes to be supported so that they are hanging down if you are not wearing shoes. This may cause the development of claw feet, which can cause problems when wearing shoes (pressure sores).
What is the best position in bed in order to avoid contractures in the hip and knee joints?
The best position is the prone position since this position stretches the joints.
Spasticity
Spasticity develops as a result of damage to the spinal cord or to the brain. The term comes from the Greek word “spasmos”, which means muscle cramp. Spasticity and spasms frequently play a central role in the lives of people with spinal cord injuries and their caretakers.
Why does spasticity occur?
The regulation of body tension is very complex. Movements are controlled jointly by the brain and the spinal cord. The spinal cord injury causes an interruption of the ascending and descending nerve paths in the spinal cord via which regulation is controlled. The brain loses its influences over reflexes and over the development of strength in the musculature.
Reflexes are involuntary movements which are controlled directly via the reflex arc in the spinal cord. The regulation of the reflexes is disrupted by the interruption to the spinal cord; they are no longer “braked”, and they respond strongly. Therefore, many people with spinal cord injuries suffer from increased muscle tone1 or cramp-like muscle activity.
Difference between spasticity and spasms
Spasticity means that the basic tone of the muscles in the paralysed parts of the body is increased. Spasms are unspecific responses to stimuli. As the central control via the spinal cord is lost, non-specific muscle contractions occur in response to sensory stimuli. A distinction is made here between flexor and extensor spasms, depending on whether the flexor or extensor muscles are more affected.
What this means to people affected
Spasticity means that the body works at the highest level of effort and results in very high energy consumption. The possible movements in the joints are restricted because the surrounding muscles are tensioned in such a way that any elasticity and, thus, the scope for movement are lost. As a result, movements take great effort which, among other things, can restrict independence. However, there are lots of positive effects to spasticity. It gives the body greater stability, causing those parts of the body which are affected by paralysis to follow the pulses of those which are not because the joints do not permit movement in any other direction due to the high tension of the surrounding muscles.
Shooting spasms may be used in a beneficial manner for performing some daily routines, e.g. during transfers where extensor spasms may enable the person to stand for a short time, to raise his or her legs up onto the bed or when getting dressing, where reflexor spasms may be useful.
If the spasms occur very surprisingly, they may also pose a risk because they may disrupt movements, leading to falls and injuries.
What this means to care personnel
Dealing with people with spasticity poses great challenges to care personnel. Care often takes great effort, for the muscle contraction of the patient can easily be transferred to the caretaker.
Key points in care
In spasticity
- People regulate their tension through movement. Therefore, frequent small changes in position are preferable to long intervals in any one position.
- When positioning the person, it is important to ensure that he or she is in a low state of tension. Fixing the legs in place in the bed generally increases body tension.
- You can put the person in a variety of possible positions in order to lower body tension. The frog and extended positions have proved to be the most effective.
In spasms
- Spasms are frequently triggered by touching. Some points of contact are more sensitive to the touch than others; they are what are known as trigger points. Trigger points include the hollows of the knees, the soles of the feet and the abdominal wall; they should be omitted during touching or should not be touched during initial contact.
- Spasms often occur very surprisingly, which can be dangerous for the people affected as well as for their caretakers. Therefore, care has to be taken with people who often experience shooting spasms. Sudden extensor spasms during transfers or reflexor spasms of the legs in bed may pose a risk to safety, whereas extensor spasms generally do not occur at a bend in excess of 90°.
Is there medication that can reduce my spasticity?
Yes. There are different groups of active substances which affect spasticity or spasms. However, they frequently have serious side effects which may also affect the ability to drive. Spasticity may only be treated with medication if it is adversely affecting daily routines such as transfers, personal care, etc.
Why does my spasticity suddenly become much worse?
This is often a warning sign that there is something wrong in the body. It could be an indication of an infection or injury.
1 Muscle tension
Read