
- 4 minutes to read
- 08 April 2021
What causes pressure sores?
Long-lasting pressure or also brief, strong pressure on one part of the skin can cause a decrease in blood flow inside the tissue. The skin presents red spots that do not turn white when pressing. Skin hardens if it is repeatedly exposed to strain at the same point.
This reddening of the skin is caused by dead cells and requires decompression. The strain needs to be alleviated. This happens specifically to body parts that are paralysed and have no sensibility. Skin often reddens in combination with shear forces and rubbing.

What are shear forces?
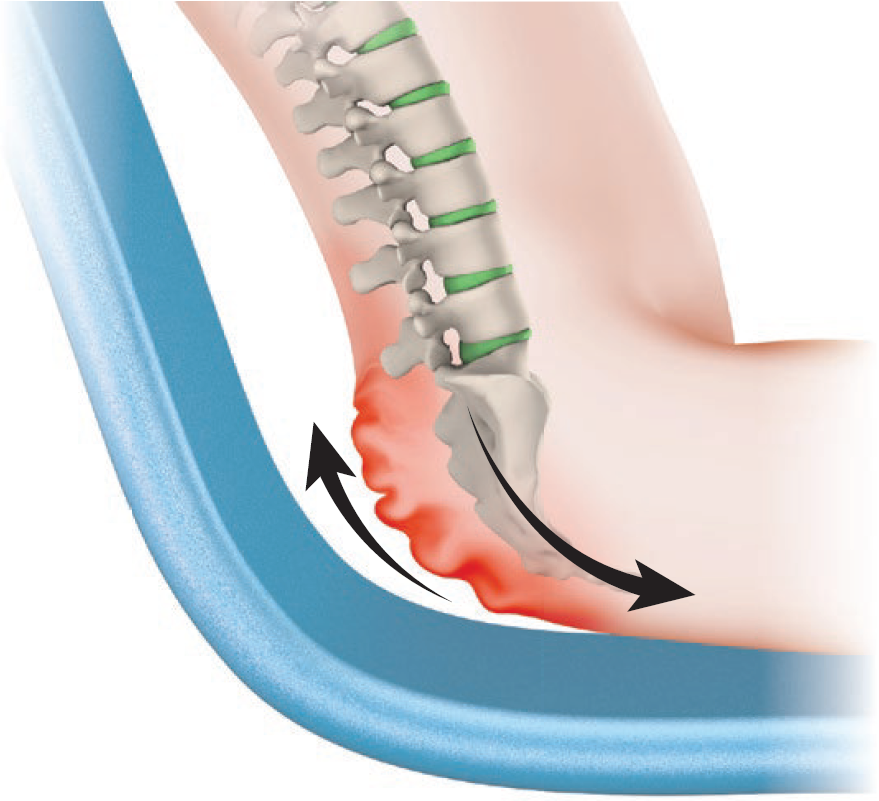
Shear forces occur when tissue is moved in opposite directions. Slow pushing or pulling of the various tissue layers causes micro injuries.
Shear forces occur when sitting in bed or when sliding over onto the wheelchair or shower wheelchair, etc.

When should the skin be checked?
The skin must be checked at least twice per day: in the morning during your personal hygiene, and at night when going to bed.
Additional skin checks are important …
… after sitting or lying on a new or unaccustomed surface
- New mattress or bedding material at home
- Unfamiliar mattress in a hotel, at friends’, in hospital, etc.
- New wheelchair or cushion
- New/unfamiliar shower seat or shower wheelchair
- Sports devices such as a monoski, handbike, speed wheelchair, etc.
- When travelling: seats on airplanes and buses, etc.
- Dentist’s chair, examination stretcher, x-ray stretcher, etc.
- Long car journeys
… after wearing new clothes and shoes
- Trousers with thick seams
… during a health condition or after an accident
- Fever, flu – attention: fever makes the skin much more sensitive!
- Diarrhoea
- Increased spasticity
- After falls
… when there are skin changes
- Swellings
- Dry skin – cracked skin, scaly skin
- Calluses
- Hard skin
… in a hot climate
- When perspiring profusely
The most important way to prevent pressure sores is to frequently check skin via visual examination and palpation:
Feeling and assessing
- Press the reddened part of the skin with your finger.
- If the spot disappears (whitish colour for 1–2 seconds), further damage can be avoided by relieving this part of the skin.
- If this part stays red, the skin is damaged and the condition is called decubitus. It is necessary to consistently relieve this part of the skin for a longer period.
- If hard skin, scabs or blisters have formed, the decubitus is deeply rooted and requires urgent treatment by a doctor.
What do I need to do in the case of pressure sores?
If reddening occurs, ease the pressure on the affected area of skin immediately until the skin has recovered. The further the pressure ulcer has progressed, the longer it will take to recover.
If an erythema can no longer be pressed away, more time is needed for the skin to recover. If the pressure ulcer occurs at a spot that is not affected when sitting in the wheelchair, it is possible to use the wheelchair during the day. However, more frequent periods of relief should be practised. If there is pressure on the affected part, it is necessary to lie in bed with frequent repositioning.
Attention: The coccyx area can also come under pressure when you are sitting in a wheelchair – shear forces.
The longer a pressure sore remains untreated, the deeper the decubitus will be and the longer the recovery period. It is not recommended to treat the wound by oneself over a longer period. Having it checked and treated by a GP or an outpatient care service helps to avoid complications.
How can I avoid pressure sores?
- Through regular relief of pressure or movement of the weight when sitting in a wheelchair – lifting, leaning to the side or ahead, tilting the wheelchair (roughly every 20 minutes)
- Pressure relief in bed by shifting into various positions – to the side, prone position
- Avoid sitting or lying by mistake on objects that can cause pressure ulcers – buttons, cell phones, etc.
- Crease-free bed sheets, suitable clothes without studs, buttons or thick seams on the buttocks or back
- By sitting on adapted cushions, if possible – on an airplane, bus, car, etc.
- Sit on a padded surface for personal hygiene: toilet seat, soft shower seat and shower wheelchair surface
If I notice a reddening at the buttocks using a mirror and cannot check myself if it can be pressed away, what can I do?
Family or a care service can hold the mirror for you or check your skin.
What do I do if I am unsure about my assessment of the reddened part?
Don’t hesitate to see your GP or ask an outpatient care service for help.
What can I do if I notice that my mattress is causing pressure sores repeatedly?
Check the age and condition of the mattress. You may have to get a softer mattress. There are various anti-decubitis mattresses available on the market. They can frequently be hired from companies on a trial basis. Ask your local SCI centre which mattresses are suitable.

Be the first to comment!