
- 6 minutes to read
- 27 January 2021
Definition of pain
Pain is a complex sensation similar to a feeling. Pain is always subjective; it cannot be measured or proven and also not rebutted. Since the 1970s there has been an official definition by the International Association for the Study of Pain which applies for acute and also for chronic pain:
"Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage."
The definition follows the bio-psycho-social model of disease. This model describes that disease – and therefore also pain – is not exclusively caused by physical changes but also dysfunction, emotional, mental or social problems and disruptions can cause pain and disease. The above definition of pain therefore dismisses the causal link of damage and pain. This means that pain is not necessarily caused by an objective damage of tissue but that a subjective sensation of such damage is sufficient.
Acute pain
In case of acute pain receptors – or, simplified, microphones or call buttons – are activated inside the body which forward their information via the spinal cord and many interfaces to the central nervous system, our brain. Inside the brain this information is processed in a complex way. The result of these processes may be the sensation of pain combined with a certain characteristic (burning, stabbing, pulling, throbbing etc.) and a more or less exact location within the body. Pain can, however, also be suppressed by the brain, e.g. when we are distracted, tense or concentrating on an interesting work or more important tasks (such as fleeing a danger, shock after an accident).
Acute pain has a warning function. The removal of the cause, treatment of the injuries or the underlying disease eases the pain mostly fast and sustainably. Painkillers usually work well.
Chronic pain
Acute pain can turn into chronic pain. Chronic associated with pain does not only mean "long lasting" or "existing for a long time". Chronic pain also includes the interrelatedness of various factors. Signs for pain that is becoming chronic are that the symptoms are spreading on the physical level – the area affected by pain is extending, more areas of pain develop – but also on the mental-emotional level and in social life problems can occur.
Chronic pain can best be prevented if it is treated early and appropriately. If it targeted and usually well working treatments have hardly any influence on the pain, it should be checked whether it is still an acute, simple pain and also other influences should be taken into consideration.
Frequent chronic pain problems are:
- Headache
- Back pain
- Neck pain
- Neuropathic pain (caused by damage of the nervous system such as spinal cord injury)
- Multilocular pain (i.e. at several locations) or extended (i.e. covering a larger body area) chronic pain (e.g. fibromyalgia)
In total about 16% of the persons residing in Switzerland are suffering from chronic pain, i.e. one in six. Persons with spinal cord injury suffer from chronic pain more frequently, often in combination with muscle spasticity. Most of them do not receive sufficient care and continue to suffer.

Causes and triggers
Pain can be versatile and each patient has a different perception of pain – as manifold can be the causes that trigger pain and they are often the beginning of several years of experiencing pain. Often the triggers occur at a time when the patient was in a difficult situation in life or has reached a turning point. Also previous injuries, experiences of violence or ongoing mental or social burdens may constitute weak points that may promote such a development.
Chronic pain, as generally recognized, can only be understood on the basis of a bio-psycho-social model of disease. The various parts may have a different significance from case to case. Chronic pain is often comes with a depressive mood, sometimes fear and often sleep disorders. In each case it needs to be examined whether sleep disorders has existed before (and may therefore have promoted the development of chronic pain) or whether they are co-existing without having an influence on the pain or whether they are the consequence of chronic pain. In each case they need to be treated in the context of a pain therapy.
Impact on the quality of life
Research in the field quality of life was able to show that chronic pain affects a person in his/her entirety and all areas of life.
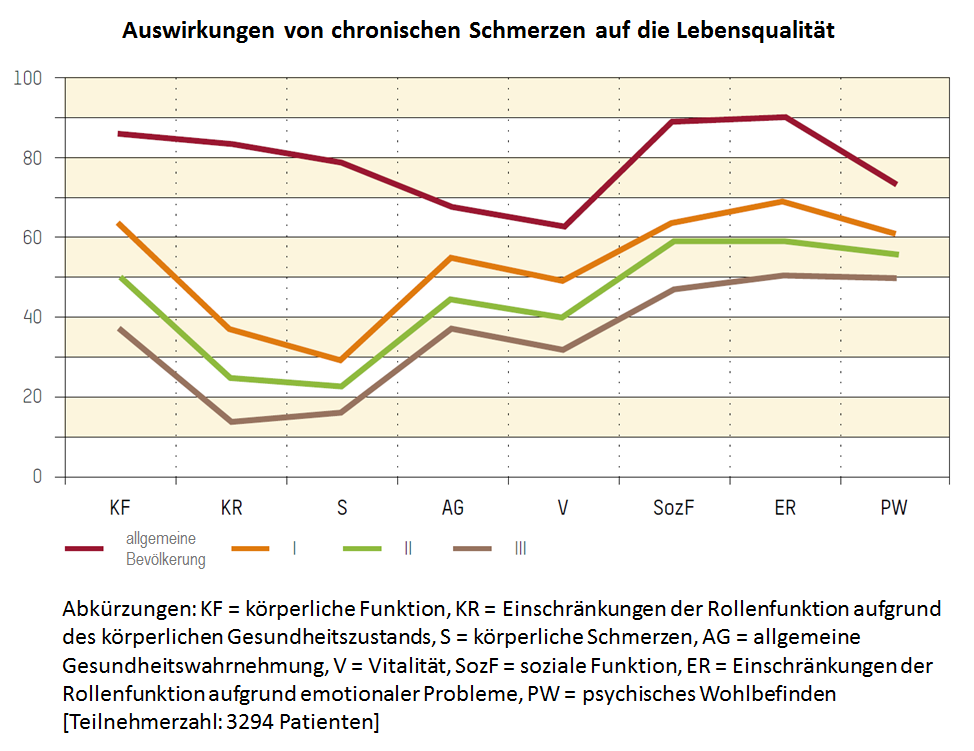
Self-assessment of health related quality of life with the SF-36 (short form 36), results in relation to pain chronification. The red curve shows the standard values of a representative sample of the general population. The orange curve "I" shows the results for patients with low chronified pain, the green curve "I" shows the values with a medium pain chronificiation and the brown curve "III" shows a high pain chronification (Mainz Pain Staging(MPSS) by Gerbershagen) [Resource: Gerbershagen HU, Lindena G, Korb J, Kramer S. Gesundheitsbezogene Lebensqualität bei Patienten mit chronischen Schmerzen. Der Schmerz. 2002;16(4),271-84.]
The diagram clearly shows that patients with an increasing pain chronification are limited in all enquired areas because of their chronic pain. Localization of the pain does not play a significant role in this context.
Diagnosis and treatment
In order to detect and diagnose chronic pain a team of specialists is necessary. An orthopedist, for example, is not able to competently assess the mood of a patient and make a psychiatric diagnosis; a social worker is not able to assess the performance of the patient, his/her limitations and resources; and a psychiatrist or psychologist cannot evaluate the degree of physical damage and the therapeutic possibilities (e.g. through physiotherapy). Therefore to assess the complexity of a patient and his/her situation, a team of pain specialists is necessary who exchange their assessments and findings and then coordinate further treatment measures. Gold standard for the treatment of chronic pain therefore is an interdisciplinary (i.e. across the disciplines) and multimodal (i.e. in different ways) pain therapy.
The success of the therapy strongly depends on the cooperation of the patient, from the anamnesis to the motivation and participation in the treatment. Generally the pain patient does not only get a diagnosis but a list of factors that causes and maintain pain. Pain is a combination of factors and gives expression to many things such as disease, suffering, limitations, suffered injustice and much more.
If possible the therapy takes place within a group since this allows the participants to support and learn from each other. In order for the group to be harmonious and for the group treatment to be successful a thorough selection of patients is necessary.
Swiss Paraplegic Centre in Nottwil, Switzerland, has the Centre for Pain Medicine, a specialist department for the treatment of acute and chronic pain. This is where outpatients and inpatients receive the best-possible examination of their pain problem and an accordingly designed treatment – see https://www.paraplegie.ch/spz/en/centre-pain-medicine-nottwil.
Useful links:
- An instructive video about how to deal with pain can be found here: www.youtube.com/watch?v=5KrUL8tOaQs.
- As a recently founded organization, "Schmerzliga Schweiz" offers information and capacity building (in German).
- A list of pain specialists with the certification "Pain specialist SASP" can be found on the website of the "Swiss Association for the Study of Pain" (SASP): www.pain.ch (in German and French).
About the author:
- Dr. med. André Ljutow, MSc, is leading the Centre for Pain Medicine, one of the biggest interdisciplinary specialist units for pain of the German-speaking countries. As "Pain specialist SASP" with numerous other international qualifications, Dr. med. Ljutow is currently also president of the Swiss Association for the Study of Pain. Furthermore, in his role on the scientific advisory board, he is working on the creation of a self-help organization for pain patients of "Schmerzliga Schweiz".

Be the first to comment!